By Nurture Connection
In June 2025, Nurture Connection hosted a conversation about the power of codesign and how parent partnership can support practice transformation in early childhood ecosystems.
Cohosted by Nicole Loveless, Nurture Connection Parent Leader and Family Network Collaborative (FNC) member, and David Willis, MD, FAAP, Founder and Director of Nurture Connection, the event included presenters Nikki Shearman, PhD, Chief of Strategic Initiatives, Reach Out and Read; Dani Dumitriu, MD, PhD, Associate Professor of Pediatrics and Director of the Center for Early Relational Health, Columbia University; and Desarae Smalls, Parent Leader from the Children’s Hospital of Philadelphia (CHOP).
Presenters shared how researchers, practitioners, and parents worked together to develop Reach Out and Read’s CONNECT Survey, a validated assessment tool for assessing the parent-clinician relationship during routine pediatric primary care. Together, they reflected on how engaging families in the research design process offers a relational foundation for implementation research and furthers the impact of Early Relational Health (ERH) promotion efforts through pediatric primary care.
Key Takeaways:
- Authentic partnerships with parents are key. Intentional codesign and collaboration builds meaningful connections, belonging, and transformation.
- Many perspectives are needed in this relational work. Codesign is a multilayered process of engaging a wide array of voices and expertise, from parents and caregivers to doctors and providers to policymakers and researchers.
- Communication starts with building common ground — approaching with nonjudgmental curiosity, acknowledging differences, trying to listen and understand each other, and using language that has shared meaning.
Bringing Family Partnership to Pediatrics
As David Willis notes, “all of this work has really come forth in terms of partnering with families.” A previous study he conducted, with Portland State University, explored parents’ perspectives on ERH in healthcare settings. Through parent-led focus groups, the study found that parents value strong relationships with their children but often experience racism, classism, and judgment from medical providers. Despite this, parents expressed a desire for healthcare providers to be more supportive and committed in promoting Early Relational Health.
This insight led to the creation of the Family Network Collaborative (FNC), a parent advisory group that helps codevelop and guide Nurture Connection’s efforts.
It also echoed a growing need in the field for a tool that could help gather direct information about the experiences that families were having in the exam room, in hopes of building better relationships between parents and providers. While many surveys existed, there weren’t any that had been designed specifically to ask parents about their experience or their relationship with their clinician during pediatric well-child visits. As Nikki Shearman shared, designing a new survey presented a unique opportunity to do this with the voice of the parents — “because the parent concepts of what makes for a good relationship, and their language, are what’s going to make this survey successful.”
Engaging Parents in Survey Design
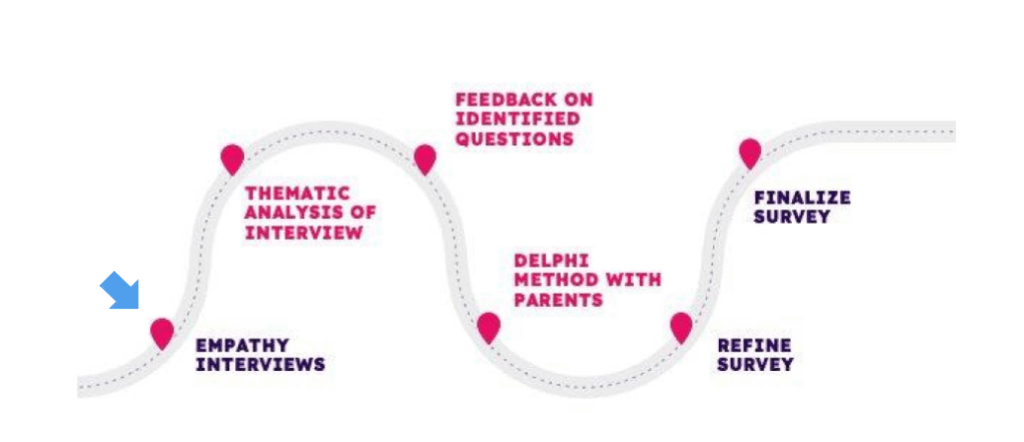
Image credit: Reach Out and Read
Parents played an integral role throughout the survey design process, which centered around exploring several core themes, including patient-centered communication, compassion and respect, and comfort and safety.
“We asked parent leaders to ask the parents around them [whom they knew] what was their well-child visit like? How did it go? What made it good? What made it bad? We took the results of that and did a thematic analysis of the interviews. We then got feedback on identified questions, and again, parents were with us the whole way.”
–Nikki Shearman, PhD
By the end of this process, they arrived at 13 questions centered around several core themes, including patient-centered communication, compassion and respect, and comfort and safety:
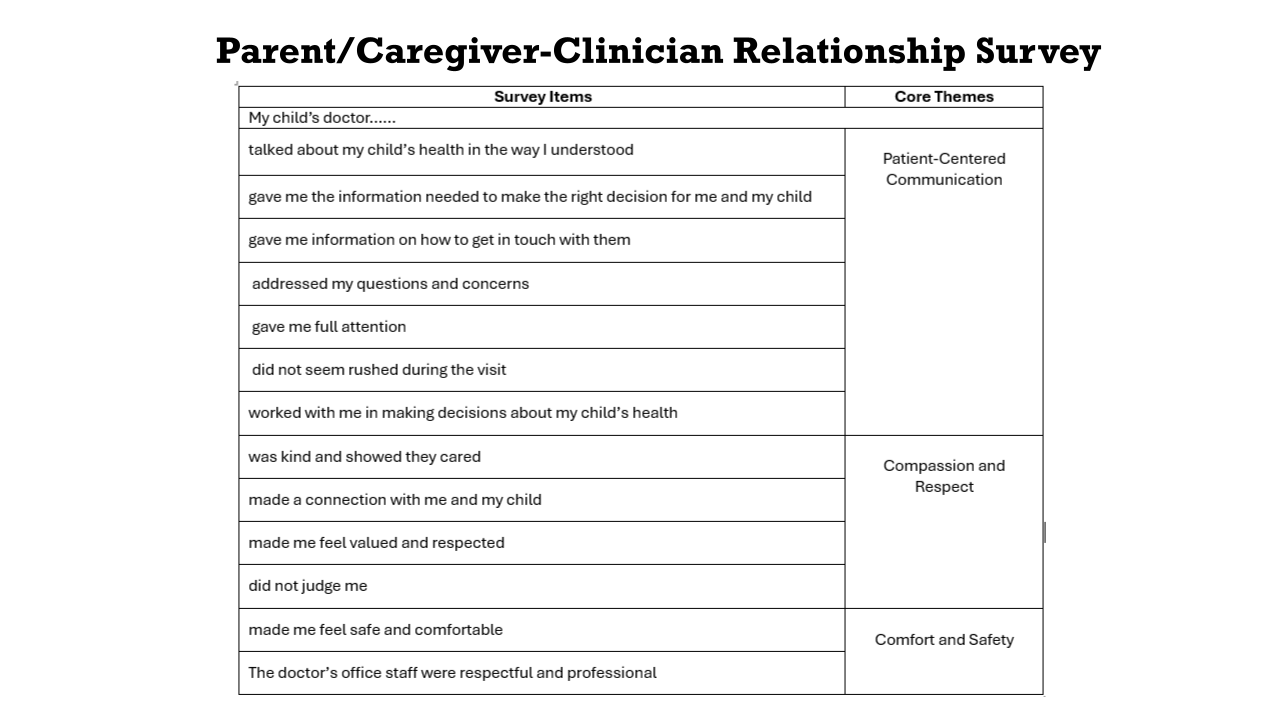
Image Credit: Reach Out and Read
Common Ground, Trust, Barriers, and Hope: Parent Leaders Reflect
Nicole Loveless and Desarae Smalls shared their experiences as parent leaders in the research process, emphasizing the importance of incorporating parent voices and addressing emotional challenges in the process.
“I really believe half of the time it’s a language barrier,” Desarae reflected. “Not everybody knows how to code-switch, or change up their language for different settings. Not everybody knows how to advocate for themselves or for their child. … It’s also a cultural barrier as well. You can’t tell people what to do. You have to go into a town and be humble enough to hear what they need.”
As Nicole notes, in addition to language and cultural barriers, historical inequity can compound these challenges of building connection: “A lot of distrust has happened in my [Native American] community as well — like the jargon, and they keep changing the systems after we have spent time trying to learn their set systems, when it’s exhausting. … We have to keep working together. We have to have hope. Otherwise, what’s the whole point of this? If we can’t even keep moving forward and have hope in this. We can’t just give up.”
They highlighted the value of using relatable language and fostering open conversations to better understand and address parents’ experiences with pediatric care.
“The Space Between”: Clinical Spaces and the Pediatrician Perspective
Dani Dumitriu also shared some insights as a pediatrician into the “space between” and factors at play in the exam room that can impact parent-provider relationships — with a particular emphasis on the relational nature of the work itself:
“In Early Relational Health, if we’re talking about ultimately being able to improve the bond between parent and child, we need to think of the other relationships in the room. If we want to help parents, we have to first improve the relationship between the parent and the doctor.”
“Ultimately, this [survey] could become something that all offices that deal with pediatric primary care, like family medicine, can use both as a benchmark to measure themselves and to put practices in place that promote the continued education of how to improve that relationship.”
Looking Ahead: The Power of Codesign
So far results from the CONNECT Survey are looking positive — showing that the survey is asking the right questions and showing us what we need to know about how parents are experiencing their well-child visits. This illustrates the importance of engaging in more codesign processes with families — by meeting them where they are and building trust between families and providers.
Showing up to hear families’ perspectives is crucial in improving pediatric care — this includes bridging clinical settings with “living room” language, hearing from different families, listening deeply, and asking questions. As Nicole encourages, “even if we don’t know the exact tools, just showing up is important.”
Explore More:
-
-
-
-
-
-
-
- Watch the webinar and check out additional resources at this link.
- Learn more about what’s next for the CONNECT Survey at this link.
-
-
-
-
-
-